Breast self-examination, or routinely inspecting your breasts on your own, can be a valuable tool for detecting breast cancer early, which in turn can help you get effective and timely treatment. While no one test can detect all breast cancers early, it is suggested that breast self-examination along with other screening measures can improve the chances of early diagnosis.
Breast self-examinations allow you to become familiar with the shape, size, and texture of your breasts. This is crucial since it can help you assess whether or not what you're experiencing is typical. Inform your healthcare practitioner if you see anything unusual in your breast.
Prepping For Self-Examination
A few days after your monthly menstrual cycle ends is the best time to undertake a breast self-exam. Because hormonal changes might alter the size and feel of your breasts, it's best to get the exam done when they're in their natural state.
Women who do not menstruate should schedule the exam on a specific day, such as the first of each month. You should also make note of your self-examinations in a journal. This will allow you to keep track of and document any changes in your breasts.
Steps For Self-Examination
Step 1: Start by looking in the mirror at your breasts with your shoulders straight and your arms on your hips. Here are some things to watch for:
• Breasts that are the same size, shape, and colour as they were before
• Breasts with a uniform shape and no obvious deformation or swelling

Please notify your physician if you notice any of the following changes:
• Skin that has dimpling, puckering, or bulging
• An inverted nipple (pushed inward instead of sticking out) or a nipple that has shifted its position
• Swelling, redness, or pain
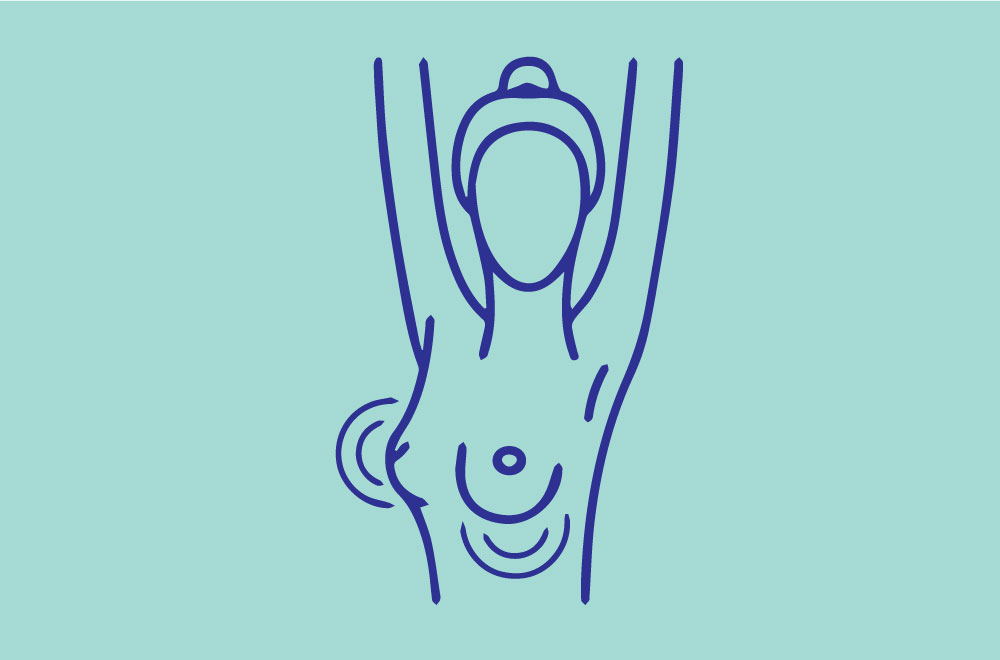
Step 2: Raise your arms now and take a closer look for the changes as stated above.
Step 3: Look in the mirror for any evidence of fluid leaking out of one or both nipples while you're there (this could be a watery, milky, or yellow fluid or blood).

Step 4: Then, while lying down, feel your breasts with your right hand on your left breast and your left hand on your right breast. Keep your fingers flat and together while applying a firm, smooth touch to the first few finger pads of your hand. Make a quarter-sized circular motion with your hands.
From your collarbone to the top of your abdomen, and from your armpit to your cleavage, cover the entire breast from top to bottom, side to side.
To ensure that you cover the entire breast, follow a pattern. You can start at the nipple and work your way outwards until you reach the outer edge of the breast. As if you were mowing grass, you can also move your fingers vertically in rows. Most women tend to respond best to an up-and-down strategy. Feel all of the tissue in your breasts, from the front to the back: light pressure for the skin and tissue just beneath; medium pressure for the tissue in the middle of your breasts; hard pressure for the deep tissue in the rear. You should be able to feel down to your ribs once you've reached the deep tissue.

Step 5: Finally, while standing or sitting, feel your breasts. Many women like to conduct this step in the shower since it is easier to feel their breasts when their skin is moist and slick. Using the same hand movements as before, cover your entire breast.

If You Find A Lump…
If you think you have a lump in your breast, don't be alarmed. Most women develop lumps or lumpy patches in their breasts at some point in their lives, and the majority of these lumps turn out to be benign (not cancerous). Non-cancerous breast lumps can be caused by a variety of factors, including natural hormonal fluctuations, a benign breast ailment, or an injury.
If you find a lump or other new and concerning breast alteration, don't hesitate to contact your doctor. This is especially true if the changes last longer than one menstrual cycle or appear to be getting bigger or more apparent in some way. When you menstruate, wait until after your period to see if the lump or other breast change goes away on its own before seeing your doctor.
Your gynaecologist, primary care doctor, or a nurse practitioner who works with your gynaecologist or primary care doctor, are the best people to call because they know you or may have done a breast exam on you before.
Your doctor will take a health history and perform a physical exam of the breast during a visit to evaluate a breast lump, and will most likely request breast imaging tests. In women under the age of 30, who are pregnant, or who are breastfeeding, ultrasound is frequently the first or only imaging test utilised to evaluate a lump.
In women over the age of 30 who are not pregnant or breastfeeding, both an ultrasound and a mammography are usually suggested to investigate a lump. Your doctor may recommend additional imaging, such as MRI (magnetic resonance imaging), MBI (molecular breast imaging), and/or a biopsy, if more testing is required. They may also refer you to an expert (usually a surgeon or oncologist) for a more thorough examination.
It's critical that your doctor explains the reason of the lump or other breast alteration, as well as a plan for monitoring or treating it, if necessary. Don't hesitate to get a second opinion if you're not satisfied with the counsel of the first doctor you see.