For millions of women across the globe, including India, recurring urinary tract infections (UTIs) are an unwelcome but familiar occurrence. Burning sensations, constant pressure, and the frequent need to urinate are common symptoms. But what happens when lab tests repeatedly come back negative, yet the discomfort persists?
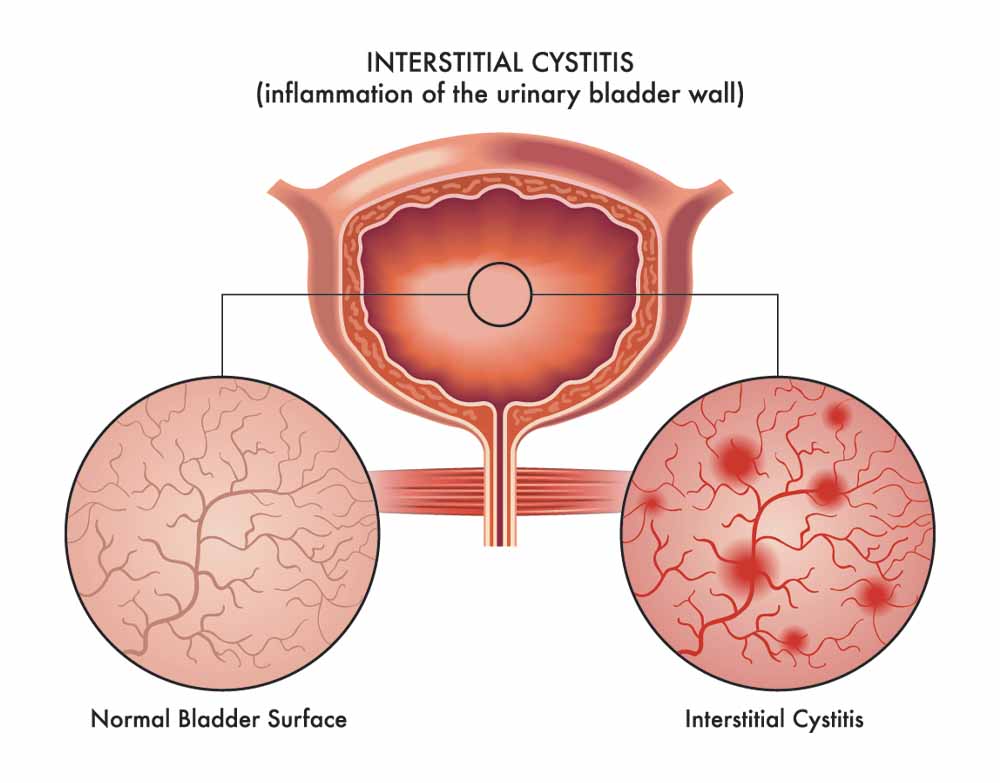
The answer may lie in a little-known and often misunderstood condition called Interstitial Cystitis (IC), also referred to as Bladder Pain Syndrome (BPS), a chronic, non-infectious inflammation of the bladder that mimics UTI symptoms but doesn’t show up in standard cultures. IC/BPS disproportionately affects women, often remains undiagnosed for years, and can deeply impact quality of life.
What is Interstitial Cystitis or Bladder Pain Syndrome?
Globally, prevalence estimates suggest that between 3–8 million women in the U.S. may suffer from IC/BPS (National Institute of Diabetes and Digestive and Kidney Diseases, USA). In India, the numbers are difficult to track due to underreporting and misdiagnosis, but recent hospital-based studies show growing prevalence among women seeking help for chronic pelvic pain. Dr. Manisha Ranjan, obstetrician-gynaecologist at Motherland Hospital, Noida, says, “We’re seeing more Indian women come in with UTI-like symptoms that don’t resolve with antibiotics. Awareness about BPS is still very low even among general physicians.”
Why Does It Get Mistaken for UTIs?

What Causes IC/BPS?
A 2022 study by AIIMS Delhi found that among women presenting with persistent pelvic pain and negative urine cultures, over 17 per cent showed symptoms aligning with Interstitial Cystitis but had never been referred to urology or pelvic pain specialists. The exact cause remains unclear, but studies point to a combination of:
• Hormonal changes, especially around menstruation or menopause
• Autoimmune reactions, where the immune system attacks the bladder lining
• Previous infections, which may have altered nerve signalling
• Pelvic floor dysfunction
• Psychological stress or trauma, including early life adversity.
Impact on Daily Life
Interstitial Cystitis goes beyond physical symptoms. According to The Journal of Urology (2018), women with IC experience higher rates of depression, sleep disturbances, and anxiety, and are more likely to report dissatisfaction in relationships and intimacy.

Common Triggers and Lifestyle Modifications
Many women find that specific foods and drinks worsen their IC symptoms. Common irritants include:
• Caffeinated drinks (coffee, tea)
• Citrus fruits
• Alcohol
• Spicy or acidic foods
• Tomatoes and soy products
A growing number of Indian hospitals now recommend keeping a bladder diary, and many urban gynaecology clinics refer patients to women’s health physiotherapists trained in pelvic floor therapy, a treatment that has shown positive outcomes in IC patients (Indian Urological Association Clinical Practice Guidelines, 2021). Additionally, some women in India have benefited from Ayurveda-inspired low-inflammatory diets, yoga, and mindfulness practices tailored to reduce pelvic tension.
Connected Conditions
IC/BPS often coexists with other underdiagnosed women’s health conditions such as:
• Endometriosis
• Irritable Bowel Syndrome (IBS)
• Fibromyalgia
• Vulvodynia

What Can You Do?
If your UTI symptoms keep coming back despite negative cultures, consider these steps:
1. See a urologist or urogynecologist with experience in pelvic pain
2. Request further testing, including cystoscopy or potassium sensitivity tests
3. Track symptoms, diet, and flare-ups in a journal
4. Avoid known irritants and consider pelvic floor physiotherapy
5. Join online forums or IC support groups for peer guidance and medical referrals
6. Advocate for a multidisciplinary treatment approach, combining urology, dietetics, physiotherapy, and mental health support.
“We need to believe women when they say something is wrong. IC is real. It’s not just in your head,” reiterates Dr. Ranjan, based on her clinical experience with urban and rural patients alike. Bladder Pain Syndrome is a serious, chronic condition that deserves medical attention, not dismissal. As awareness slowly grows across India, more women are finding validation, relief, and long-term management options that improve their lives, physically, emotionally, and socially.