When it comes to menstrual health, terms like endometriosis have increasingly entered the mainstream, thanks to growing awareness and advocacy. But another equally common and painful condition, adenomyosis, remains shrouded in silence, leaving countless women undiagnosed, untreated, and often feeling ignored. Dr. Ananya Rao, a gynaecologist specialising in chronic pelvic pain, emphasises the importance of better awareness: “Adenomyosis is not rare. It’s just rarely talked about. We need to empower women to recognise when their periods are abnormal, to seek help, and to demand a thorough investigation. Just because heavy periods are common doesn’t mean they’re normal or healthy.”
What is Adenomyosis?
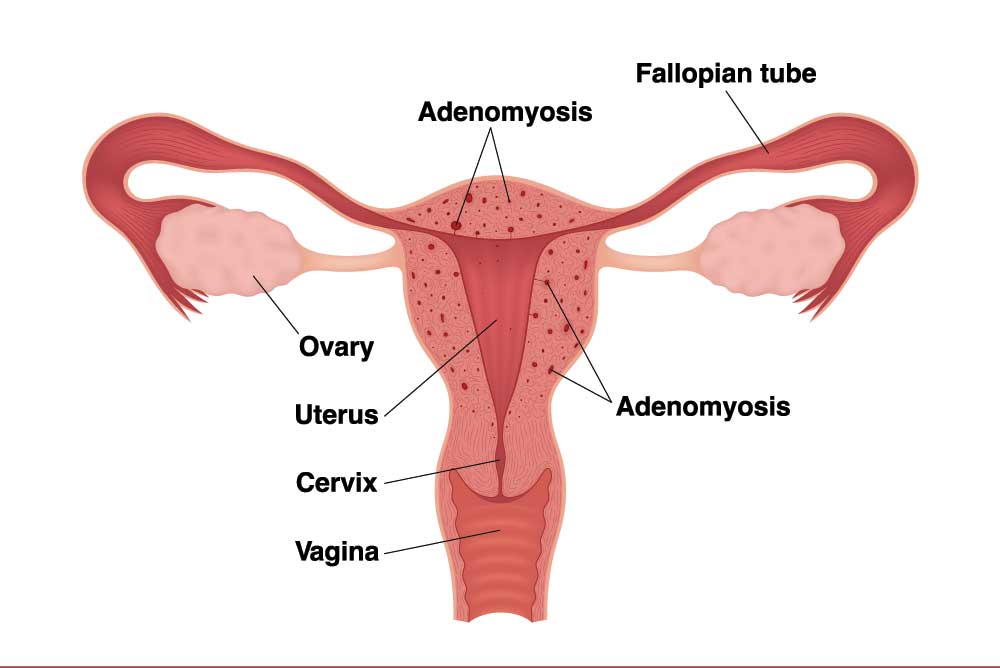
Adenomyosis is a gynaecological condition where the tissue lining the inside of the uterus (the endometrium) grows into the muscular wall of the uterus (the myometrium). This abnormal growth causes the uterus to become enlarged and inflamed, leading to heavy or prolonged menstrual bleeding, severe cramps, bloating, pelvic pressure, and fatigue.
Many women describe the pain as debilitating, often requiring them to miss work, social events, or even basic daily tasks. Unlike regular menstrual discomfort, adenomyosis pain doesn’t always confine itself to the days of one’s period, it can extend across the cycle, leaving sufferers in near-constant discomfort.
Adenomyosis vs. Endometriosis
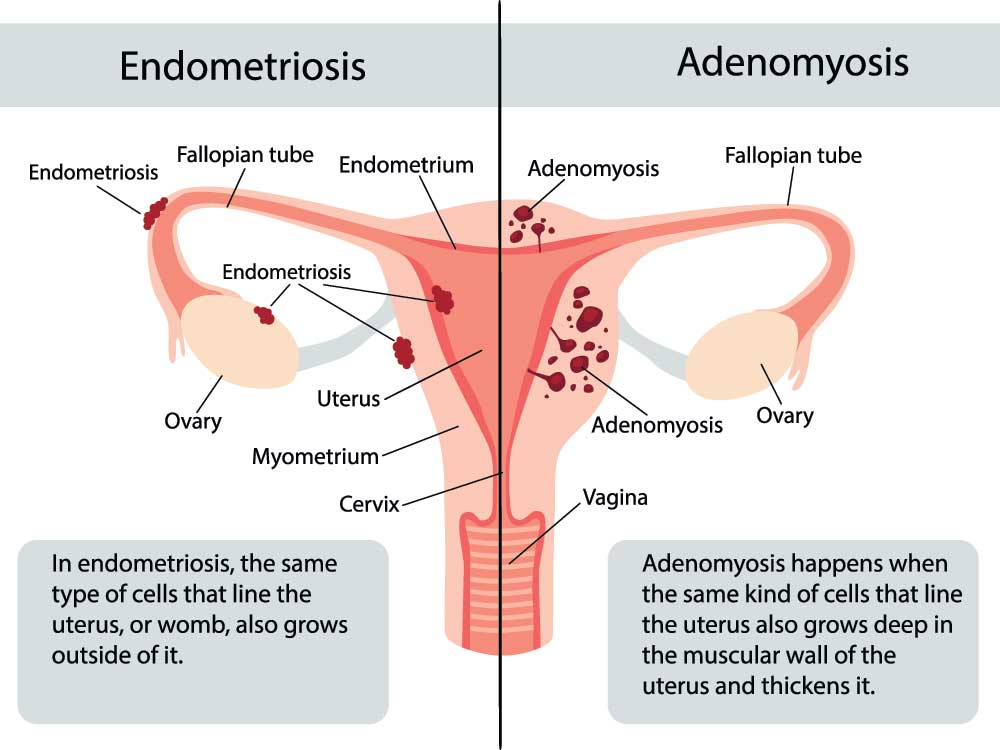
Although adenomyosis and endometriosis share similarities, they are distinct conditions. Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often on the ovaries, fallopian tubes, or pelvic lining, causing pain, infertility, and adhesions.
Adenomyosis, in contrast, involves the tissue growing into the uterine muscle. Both conditions can coexist, making diagnosis even more complex. Importantly, while endometriosis has gained significant awareness, adenomyosis remains under-researched and under-discussed, despite the suffering it causes.
How Common Is It, Especially in India?
Globally, up to 1 in 10 women may have adenomyosis—that’s roughly the same prevalence as endometriosis. But what about India?
Studies across India show varying prevalence rates, especially among women undergoing hysterectomy for abnormal uterine bleeding (AUB). For example, a study at Mahatma Gandhi Medical College & Research Institute in Pondicherry found that 55.6 per cent of hysterectomy specimens showed adenomyosis (International Journal of Reproduction, Contraception, Obstetrics and Gynaecology). Another study from Kozhikode, Kerala, reported a 16.8 per centprevalence among similar patients (International Journal of Research in Medical Sciences). A broader South India study found an overall prevalence of 23.5 per cent in hysterectomy specimens (Journal of Clinical and Diagnostic Research).
Most cases are reported among women aged 41–50 years, placing the condition squarely within the perimenopausal population in India. Common symptoms include abnormal uterine bleeding (seen in up to 92 per cent of cases), dysmenorrhoea, and chronic pelvic pain, although, notably, 7 per cent of women were asymptomatic.
Despite these significant numbers, awareness among Indian women remains startlingly low, reflecting a global trend of neglect around this condition.
The Symptoms Women Are Told to Ignore

Heavy periods? That’s just part of being a woman. Crushing pelvic pain? Take a painkiller. Bloating and fatigue? You’re probably just stressed.
Sound familiar? Women are often socialised to downplay or normalise pain, especially menstrual pain. This normalisation creates a dangerous blind spot: conditions like adenomyosis are dismissed as “just bad periods” or written off as hysteria or exaggeration.
This culture of minimising women’s pain is known as female pain bias. It’s the reason so many gynaecological conditions go undiagnosed, why women are less likely to be given pain relief in emergency rooms, and why their health concerns are often trivialised.
Why Aren’t We Talking About It?

There are several reasons why adenomyosis has remained in the shadows. Firstly, medical research has historically prioritised male bodies, leaving many female-specific conditions under-studied. Secondly, there’s a lack of clear, non-invasive diagnostic tools, making it hard to track and study the condition systematically.
Culturally, menstruation itself remains a taboo subject in many societies, including India, cloaked in shame and silence. This stigma makes it harder for women to speak openly about their periods, let alone challenge medical dismissals of their symptoms.
In short, we don’t talk about adenomyosis because we don’t talk enough about women’s pain, periods, or reproductive health in general.
Treatment Options
There is no one-size-fits-all treatment for adenomyosis. Options range from symptom management to surgical intervention, depending on the severity and the woman’s reproductive goals.
Hormonal treatments: Birth control pills, hormonal IUDs, and gonadotropin-releasing hormone (GnRH) agonists can help regulate periods and reduce symptoms, though they don’t eliminate the disease.
Pain management: Non-steroidal anti-inflammatory drugs (NSAIDs) can offer some relief, but many women find them insufficient.
Surgical options: For severe cases, surgical procedures such as endometrial ablation, uterine artery embolisation, or, in extreme cases, hysterectomy (removal of the uterus) may be recommended.
Unfortunately, as adenomyosis is often diagnosed only after hysterectomy, many women endure years of trial-and-error treatments before receiving definitive relief.
Why Awareness Matters
Raising awareness about adenomyosis isn’t just about medical accuracy but improving quality of life. Women deserve to understand their bodies, have access to accurate diagnoses, and receive effective, compassionate care.